The Spanish Flu in the Netherlands. Like A Scythe Across the Country
One hundred years ago the world encountered a Spanish flu pandemic which cost an estimated 50 to 100 million lives. That is many times the death toll of World War I, in whose wake the disease arose. It was the greatest and most deadly disease since the plague in the middle ages. But in the Netherlands it was long underestimated by the government. Medical historian Leo van Bergen sketches the devastation caused by Spanish flu between 1918 and 1920.
In his Dagboeknotities van een landstormman (Journal of a soldier), writer-solider A.M. de Jong included a few remarks regarding the Spanish flu which had relegated around 40,000 of his 200,000 fellow soldiers to sickbeds in July-August 1918. It was the first, least deadly wave, and so he was still able to speak of it with a mix of cynicism and lightheartedness. Firstly, this time, once again, the brave Dutch soldier would succeed in pushing the Spanish invader over the border, and secondly, the flu was a pleasant way of legally shirking duty. This trivialising tone was to disappear completely in his work Frank van Wezels roemruchte jaren (Frank van Wezel’s illustrious years), written in 1928. The second wave left no space for humour. ‘This time,’ he wrote literally, ‘it was not a matter for irony.’
Soldiers were repeatedly brought from the city or surrounding area to the hospital, delirious with high fever, and the sickness moved at lightning speed, corroded the lungs and in a couple of days, sometimes in a matter of hours, dragged the young life to the grave. (…) Afternoon hospital arrivals died at night. One after another, dozens in a week.
Mass death
How right he was. October and November 1918 were the deadliest months in Dutch history, with more than 20,000 more deaths than in the same months of 1917, and that in a population of 6.5 million. Of those, around 10,000 were diagnosed with ‘Spanish flu’. Altogether in the brief two years in which the influenza ravaged the Netherlands (first wave, July-August 1918; second wave, autumn 1918 to spring 1919; third wave, spring 1920) more than 20,000 people died as a direct result and another 10,000 to 30,000 indirectly, as a result of complications. When we include the colonies of the time, the figure rises dramatically. The current estimation for the Dutch East Indies is between 1.5 and 2 million, or 1 in 30-40 of the approximately 60 million inhabitants at that time.
A ‘mild’ illness
A good month after newspaper reports first appeared of ‘a secretive sickness’ in Spain, at the start of July 1918 the virus crossed the border near the German town of Emmerich. The disease spread across the country in no time, with reports from Groningen to Maastricht. The numbers were worrying, but did not yet reveal the full seriousness of the matter, although deaths were soon reported and the enormous speed with which the disease spread was a source of anxiety, as was the fact that it was not only children and the elderly who seemed to be affected, but also people aged between 20 and 50. The prevailing story, however, remained that it was a ‘mild’ illness; just ‘the flu’. Moreover the Dutch position of neutrality would improve the citizens’ resilience in comparison with the warring countries. The optimists seemed to be right. After a few weeks the worst seemed to be over. In August, 534 Dutch people died of it, in September 183; and those were ‘old cases’. But the worst was yet to come. From the end of September there was no further question of underestimation. The second wave swept across the country like a scythe.
 Press illustration from a Dutch daily newspaper, circa 1918-1919, which reads: Spanish flu is rampant.
Press illustration from a Dutch daily newspaper, circa 1918-1919, which reads: Spanish flu is rampant.No accumulation of people
In mid-July the Central Health Council issued a communiqué in which ‘Spanish flu’ was elevated to the official designation and in which people were urged to employ good hygiene and fresh air, visit their doctor promptly and avoid contact with the sick. The council also advised the avoidance of ‘accumulation of people’ as far as possible. This hesitant, relatively inactive attitude continued to be typical during the second wave too. After all, nothing was known about this form of influenza. People were groping in the dark when it came to the cause and means of transmission, as well as options for prevention and cure. A national state of emergency was therefore never declared.
The only concrete measure the government took was to increase bread rations in mid-November – from 200 to 280 grams per person per day. The official reason for this was that it would increase resilience in the population. It was also said that no miracles could be expected, as even the healthy could succumb to this strain of influenza, which suggests that this was more about reducing the risk of social unrest, which had previously culminated in a failed social revolution. Viewed alongside the war itself, the new stream of refugees and the arrival of Willem II, that social unrest explains why the influenza did not receive the government attention it clearly deserved based on its calamitous consequences. It was noteworthy that the Orange victory march after the failed revolution missed out the northern provinces. Officially this was because of the influenza, but those provinces were also socialist strongholds. Moreover their own advice to avoid crowds was thrown to the wind. On 17 November 15,000 Catholics assembled in Amsterdam and the next day in The Hague 40,000 Orangists of all faiths celebrated.
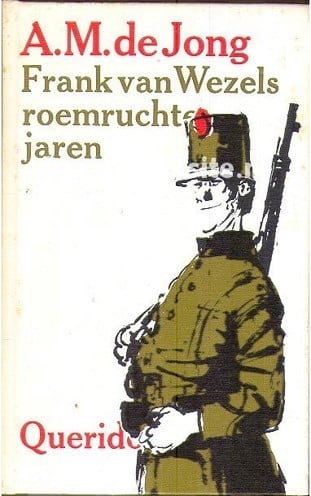
 A military hospital in Kansas during the Spanish flu pandemic in 1918
A military hospital in Kansas during the Spanish flu pandemic in 1918© The National Museum of Health and Medicine, Armed Forces Institute of Pathology, Washington, D.C., United States
Social life goes silent
In contrast the municipal measures came down to complying with advice to avoid crowds. Cinemas were closed. Fairs were cancelled, as were theatrical and musical performances, not least because the actors and musicians had taken to their beds. In many cases schools were closed, although it was Amsterdam, the largest city in the country, which omitted to do this. Even there, though, keeping children at home was not treated as ‘unauthorised truancy’ during that period.
Amsterdam did not take actions such as closing the schools for fear of stopping social life, although that had largely ground to a halt anyway. The fire brigade, tram and telephone service were disrupted. Banks struggled with staff shortages. Even the Onze Lieve Vrouwe Gasthuis hospital had to close its doors. Too many patients, too few nurses and doctors.
 Onze Lieve Vrouwe Gasthuis hospital in Amsterdam
Onze Lieve Vrouwe Gasthuis hospital in AmsterdamSchools were closed in cities such as The Hague and Rotterdam. This seemed to have a positive effect, but after a few months, Rotterdam’s death rate was actually (somewhat) higher than that of Amsterdam. The most obvious reason was the difference in prosperity and associated living conditions. Closer examination of The Hague confirms this. There, the residents had the most spacious houses and the death rate was the lowest. The greater the space in living quarters, one doctor noted in early August, the lower the chance of infection.
Slaughter in the east
This is confirmed by the enormous number of deaths in the east of the country, with its large, poor families in small ‘houses’. In October 124 people died in Almelo, compared with 11 in October 1917. In Enschede the death toll rose above 30 people per week, compared with 10 normally. But there were several causes. In Drenthe, for example, it seems that, paradoxically enough, increased wealth resulting from the war was an additional culprit. Due to the lack of coal from Germany, peat from Twente became more popular and more expensive. This attracted unemployed labourers, only increasing overpopulation and the average level of poverty when the influenza struck. Furthermore, it involved people in a relatively substantially affected age group, an effect amplified by border workers remaining at home out of fear of falling ill in Germany.
There was almost no aid. An appeal by the mayor of Emmen to the University of Groningen received just two responses from medical students, in part because others were in Limburg supplying medical aid to refugees. The end of the war did make it possible to deploy a handful of reserve officers, although this did little to change the death toll. In Emmen, 366 people died in November, compared with 26 a year before. Grave diggers had to be supported by labourers, who themselves were constantly drunk because they too, like the soldiers, thought that alcohol prevented infection.
Powerless medics
The medics were at a loss, although there was no lack of discussion about the illness. Debate, however, focused on the suspected cause, to such an extent that one doctor eventually made an appeal for a search for the only thing of importance: a cure. That remained illusive, however. They came no further than recommendations as to sensible behaviour: breathing through the nose, washing hands, walking, bed rest and … smoking plenty ‘because it keeps the mouth closed’.
 Advertisement for hot Indian spices to cure the Spanish Flu
Advertisement for hot Indian spices to cure the Spanish FluThe most important regular medical recommendation, however, was this: don’t be fooled by advertisements promising prevention or cure. In July 1918 this protest even led to the decision of the Algemeen Dagblad no longer to publish such advertisements. Remedies such as antiseptic mouthwash, hot Indian spices, beetroot (‘guaranteed effective!’), the ‘electro-homeopathic’ remedy of the – non-existant – Italian Count Mattei, or, the most famous, abbey syrup. At least the latter two were eradicated by the Vereniging tegen Kwakzalverij (Association against Quackery).
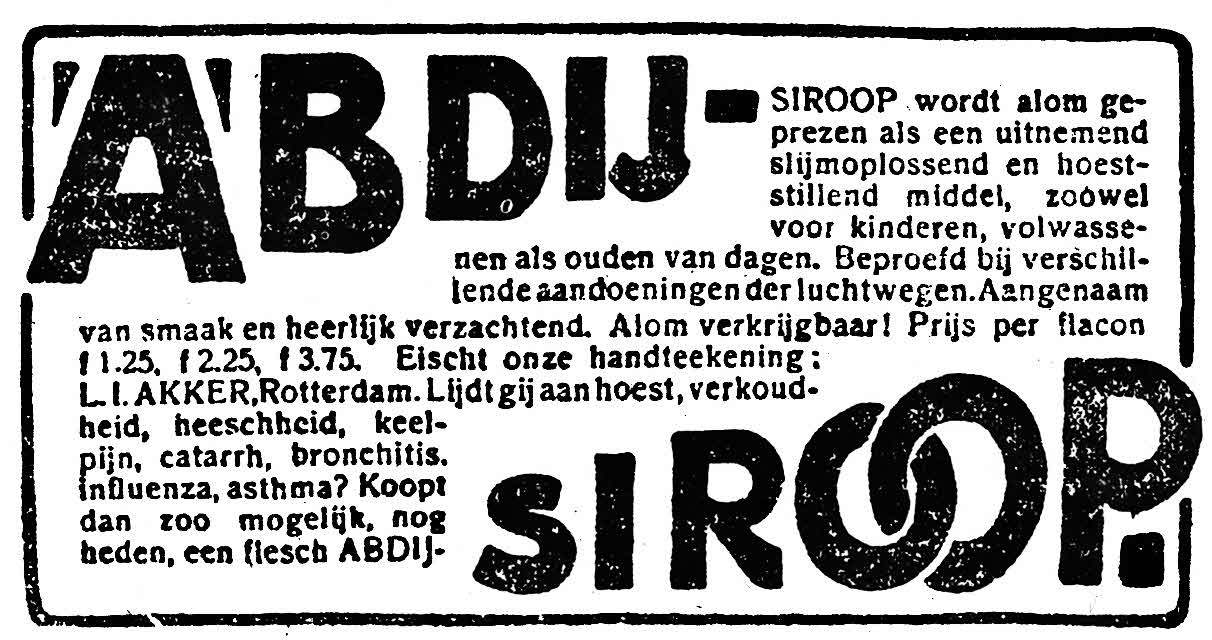 Advertisement for abbey syrup to cure the Spanish Flu
Advertisement for abbey syrup to cure the Spanish FluThe most important regular medical recommendation, however, was this: don’t be fooled by advertisements promising prevention or cure. In July 1918 this protest even led to the decision of the Algemeen Dagblad no longer to publish such advertisements. Remedies such as antiseptic mouthwash, hot Indian spices, beetroot (‘guaranteed effective!’), the ‘electro-homeopathic’ remedy of the – non-existant – Italian Count Mattei, or, the most famous, abbey syrup. At least the latter two were eradicated by the Vereniging tegen Kwakzalverij (Association against Quackery).
The boundary between regular medicine and quackery, however, was vague. Even general practitioners – out of desperation and the drive to experiment – prescribed unproven remedies which would normally never be deployed, such as ‘sublimaat’ (a compound of chlorine and mercury) or ‘collargol’ (colloidal silver). Most, however, were aware of their powerlessness and simply worked to combat the symptoms as best they could, with the help of painkillers, fever-lowering remedies and if necessary a generous dram to stop the chills. In that respect the peat workers and the soldiers were therefore in good company, even if they were using the spirits for prevention rather than cure.
The birth of H1N1
The influenza was a dramatic, but forgotten period in recent international Dutch history, also because it has long been said that it was completely separate from the war. Whether that period was more dramatic or in fact less so than in neighbouring countries, it is difficult to say due to lack of data from the countries at war. But what is clear is that Western Europe came off relatively lightly compared with the carnage in some countries in Africa and Asia.
 A colorized image of the 1918 virus taken by a transmission electron microscope (TEM).
A colorized image of the 1918 virus taken by a transmission electron microscope (TEM).Photo © Cynthia Goldsmith
The flu disappeared as fast as it came. After the resurgence in 1920, which has not even been established with any certainty to be the same strain, life in the Netherlands returned to normal and the attention of the people returned to more run-of-the-mill matters: football, hunger, war, rising dictatorships. Medically, however, the subsequent years would demonstrate two things which might have placed the flu period – which the medics, too, wanted to forget as quickly as possible – in a different, and for them altogether more glorious light. A mould named penicillin that ate bacteria was detected in a Petri dish. At around the same time it was discovered that in addition to bacteria even smaller pathogens existed: viruses. Influenza was a virus, and the strain that had caused the pandemic of 1918-1919, which had wrought such death and destruction, had the honour of opening up the sequence of diverse variants. The pandemic was over and the virus type H1N1 was born. Many variants would follow.